Pacifier and colic: What’s the connection?
Pacifier and colic: What’s the connection?
Post Author
Post Author

Megan N. Freeland, PharmD
Content Writer
Medically reviewed by
Medically reviewed by

Dr. Marcy Borieux, MD, FAAP
Pediatrician

Dr. Leo Damasco
Pediatrics and Emergency Medicine



No matter where you fall on the spectrum of opinions, there’s a good chance you’re interested in using a pacifier with your baby, especially if you have a baby who cries a lot or is difficult to soothe. Read on to find out more about pacifiers, their connection to colic, and how they can be helpful when you’re trying to get your baby to sleep.
Understanding infantile colic in newborns
Before we dive into pacifiers, let’s discuss colic. If there’s one thing newborns and infants are notorious for, it’s crying. A baby with infantile colic, often described as a “colicky baby, ”cries more than usual, seemingly for no apparent reason.
You may have heard of the 3-3-3 rule (also known as the rule of threes). It’s a common guideline for identifying colic: a baby is considered colicky if they cry for at least 3 hours a day, at least 3 days a week, for at least 3 consecutive weeks.
If your newborn develops colic, you’ll typically start to notice the symptoms between 3 and 6 weeks of age. The good news is that colic often begins to ease up when your baby is about 3 to 4 months old.
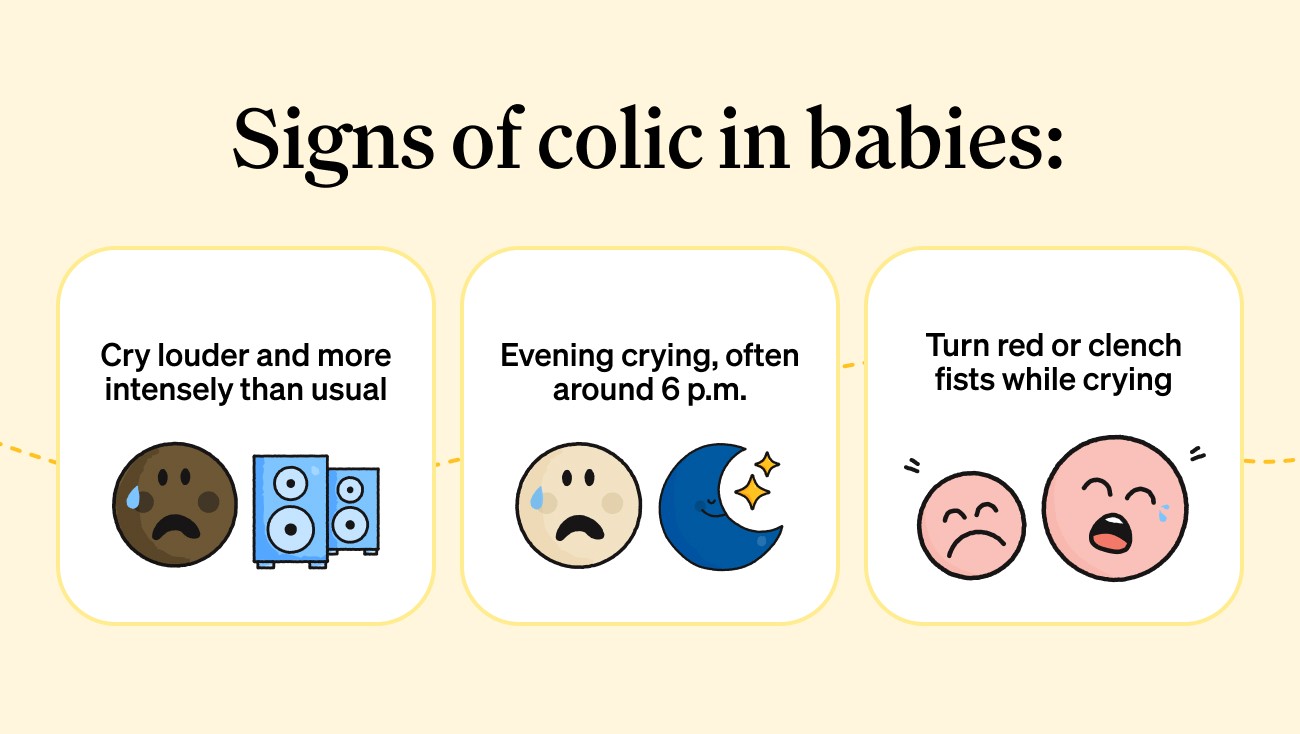
Symptoms of colic
Babies with colic may show the following signs:
Cry louder and more intensely than typical newborn cries.
Cry more frequently in the evening hours, often starting around 6 p.m.
Appear red-faced or clench their fists while crying.
While gassiness doesn’t cause colic, colicky babies may swallow air while crying, which can lead to extra gas and frequent burping. You might wonder if burping could help relieve colic symptoms by reducing gas buildup, but a 2015 study found that babies who were routinely burped didn’t experience fewer colic episodes.
How to calm a newborn with infantile colic
If you’re baby is showing signs of colic, the first step is consulting your pediatrician to check for underlying medical conditions (like reflux) to explain why your baby is crying.
Beyond identifying possible medical causes, here are several different ways to soothe a newborn with colic:
Skin-to-skin: Skin-to-skin contact with a parent can help calm your newborn.
Motion: Going for a drive, a walk in the stroller, or placing your baby is a baby carrier.
Baby massage: A gentle massage may help your baby relax and feel more calm.
Swaddling: Babies like to be held close, and a snug swaddle can help babies feel safe and soothed.
White noise: White noise can be soothing for babies during the day and night.
Colic carry: Holding your baby tummy down on your forearm while supporting their head with your hand is known as the “colic carry” or “colic hold.”
Breastfeeding: Nursing your baby provides close contact with mom and reinforces their sucking reflex, both of which can be comforting to your baby.
Pacifiers: The sucking motion of a pacifier can be soothing.
Using pacifiers to calm a colicky newborn
The main purpose of a pacifier is to help babies self-soothe by engaging their natural sucking reflex. This newborn reflex allows newborns to feed, whether from the breast or a bottle, but it also plays an important role in comfort. Babies often use the same sucking motion when they suck on a thumb or pacifier, and this repetitive action can have a calming, soothing effect, especially for babies who are fussy or colicky.
What are the benefits of pacifiers for babies?
When babies suck on a pacifier, their thumb, or any other object without getting milk, it’s called non-nutritive sucking. This natural behavior can be beneficial for babies’ growth and development, especially for babies born prematurely.
Research on preterm infants shows that non-nutritive sucking can help them transition more easily to feeding by mouth and may even shorten their hospital stay. It also helps babies self-soothe, reduces stress, and strengthens the muscles needed for feeding. For these reasons, many pediatricians introduce pacifiers to preterm babies soon after birth.
Beyond supporting growth and development, pacifiers offer several additional benefits, such as:
Lowering the risk of sudden infant death syndrome (SIDS)
Soothing fussy or colicky babies
Helping babies fall asleep
Why some doctors don’t recommend pacifiers
While pacifiers have several benefits, they can also pose some risks. Some of the potential drawbacks include:
Breastfeeding challenges: Using a pacifier too early may cause “nipple confusion” and make it harder for some newborns to establish effective breastfeeding.
Dental problems: Prolonged pacifier use, especially beyond the first couple of years, can affect dental development and lead to misaligned teeth.
Increased risk of infections: Pacifiers may contribute to ear infections and thrush, a common yeast infection that occurs in the mouth.
When should I introduce a pacifier to my baby?
The best time to introduce a pacifier depends on your baby’s individual needs and feeding situation.
Breastfed babies: Wait until around 1 month of age, after breastfeeding and latching are well established, before introducing a pacifier. In some cases, your pediatrician may recommend starting sooner if your baby is nursing effectively and gaining weight.
Bottle-fed babies: Babies who drink breast milk or formula from a bottle can typically be introduced to a pacifier at any time, since they don’t need to establish a breastfeeding routine.
Preterm babies: For premature infants, pacifiers can be especially helpful. Non-nutritive sucking supports growth, development, and helps them better transition to oral feeding.
When introducing a pacifier, look for:
The right size, according to your baby’s age.
Pacifiers with one piece, not multiple pieces.
A pacifier that’s easy to clean.
Do pacifiers lower the risk of sudden infant death syndrome (SIDS)?
Pacifier use has been linked to a lower risk of SIDS, which is most common in babies under one year old. Experts aren’t entirely sure why pacifiers reduce SIDS risk, but a few theories exist. One possibility is that babies don’t sleep as deeply when using a pacifier, making it easier for them to wake up if there’s a breathing issue. Another theory is that the pacifier’s position helps keep the tongue forward, preventing it from blocking the airway.
If you have questions about colic or pacifier use, reach out to your local or Summer Health lactation specialist for support. Summer Health is a pediatric telehealth platform offering 24/7 care, providing answers for everything from urgent concerns to everyday questions about your child’s health.

FAQs
What’s the best type of pacifier for babies with colic?
There’s no specific “colic pacifier” proven to treat colic, but certain features improve soothing, such as:
Orthodontic nipple shape: Supports natural palate oral development and is easier to keep in the mouth.
One-piece silicone design: Safer (no seams or parts that can break), easier to clean, and recommended by the American Academy of Pediatrics (AAP).
Soft, flexible medical-grade silicone: May be more comfortable for fussy or colicky infants.
Lightweight shield: Pacifiers with lightweight shield better stay in the mouth, which can be especially helpful with younger infants who fatigue easily.
What’s the best way to clean a pacifier?
Clean your baby’s pacifier with warm water and gentle dish soap. Some pacifiers can be sterilized as well. Always follow the manufacturer’s cleaning instructions for best and safest results. Do not use a pacifier that is damaged.
Is it safe to dip a pacifier in honey or juice?
It is not safe to dip your baby’s pacifier in honey or juice. Honey is dangerous for babies under one year, as it may be contaminated with toxic bacteria called Clostridium botulinum, which may cause infant botulism. Infant botulism is a serious life-threatening disease which can cause damage to the nervous system and death. Additionally, babies do not need sugar from juice, which may also reinforce unhealthy habits and cause oral health issues.
No matter where you fall on the spectrum of opinions, there’s a good chance you’re interested in using a pacifier with your baby, especially if you have a baby who cries a lot or is difficult to soothe. Read on to find out more about pacifiers, their connection to colic, and how they can be helpful when you’re trying to get your baby to sleep.
Understanding infantile colic in newborns
Before we dive into pacifiers, let’s discuss colic. If there’s one thing newborns and infants are notorious for, it’s crying. A baby with infantile colic, often described as a “colicky baby, ”cries more than usual, seemingly for no apparent reason.
You may have heard of the 3-3-3 rule (also known as the rule of threes). It’s a common guideline for identifying colic: a baby is considered colicky if they cry for at least 3 hours a day, at least 3 days a week, for at least 3 consecutive weeks.
If your newborn develops colic, you’ll typically start to notice the symptoms between 3 and 6 weeks of age. The good news is that colic often begins to ease up when your baby is about 3 to 4 months old.
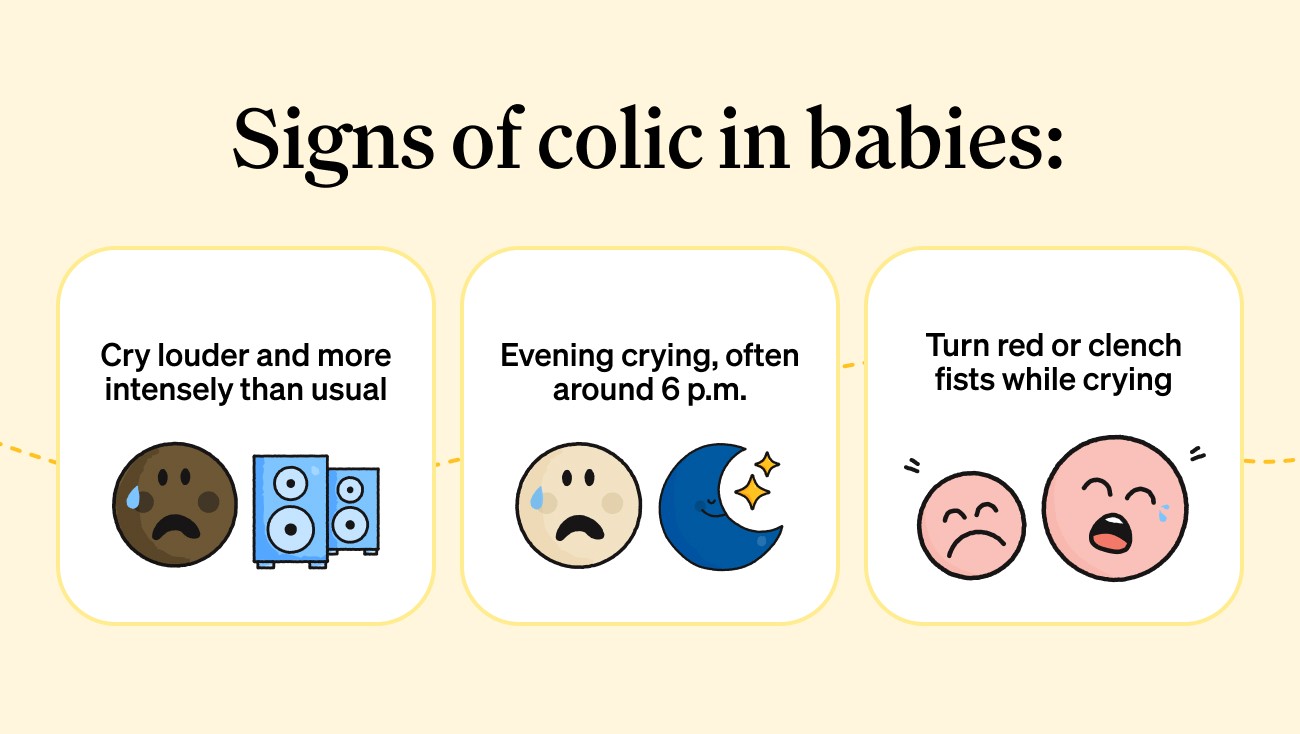
Symptoms of colic
Babies with colic may show the following signs:
Cry louder and more intensely than typical newborn cries.
Cry more frequently in the evening hours, often starting around 6 p.m.
Appear red-faced or clench their fists while crying.
While gassiness doesn’t cause colic, colicky babies may swallow air while crying, which can lead to extra gas and frequent burping. You might wonder if burping could help relieve colic symptoms by reducing gas buildup, but a 2015 study found that babies who were routinely burped didn’t experience fewer colic episodes.
How to calm a newborn with infantile colic
If you’re baby is showing signs of colic, the first step is consulting your pediatrician to check for underlying medical conditions (like reflux) to explain why your baby is crying.
Beyond identifying possible medical causes, here are several different ways to soothe a newborn with colic:
Skin-to-skin: Skin-to-skin contact with a parent can help calm your newborn.
Motion: Going for a drive, a walk in the stroller, or placing your baby is a baby carrier.
Baby massage: A gentle massage may help your baby relax and feel more calm.
Swaddling: Babies like to be held close, and a snug swaddle can help babies feel safe and soothed.
White noise: White noise can be soothing for babies during the day and night.
Colic carry: Holding your baby tummy down on your forearm while supporting their head with your hand is known as the “colic carry” or “colic hold.”
Breastfeeding: Nursing your baby provides close contact with mom and reinforces their sucking reflex, both of which can be comforting to your baby.
Pacifiers: The sucking motion of a pacifier can be soothing.
Using pacifiers to calm a colicky newborn
The main purpose of a pacifier is to help babies self-soothe by engaging their natural sucking reflex. This newborn reflex allows newborns to feed, whether from the breast or a bottle, but it also plays an important role in comfort. Babies often use the same sucking motion when they suck on a thumb or pacifier, and this repetitive action can have a calming, soothing effect, especially for babies who are fussy or colicky.
What are the benefits of pacifiers for babies?
When babies suck on a pacifier, their thumb, or any other object without getting milk, it’s called non-nutritive sucking. This natural behavior can be beneficial for babies’ growth and development, especially for babies born prematurely.
Research on preterm infants shows that non-nutritive sucking can help them transition more easily to feeding by mouth and may even shorten their hospital stay. It also helps babies self-soothe, reduces stress, and strengthens the muscles needed for feeding. For these reasons, many pediatricians introduce pacifiers to preterm babies soon after birth.
Beyond supporting growth and development, pacifiers offer several additional benefits, such as:
Lowering the risk of sudden infant death syndrome (SIDS)
Soothing fussy or colicky babies
Helping babies fall asleep
Why some doctors don’t recommend pacifiers
While pacifiers have several benefits, they can also pose some risks. Some of the potential drawbacks include:
Breastfeeding challenges: Using a pacifier too early may cause “nipple confusion” and make it harder for some newborns to establish effective breastfeeding.
Dental problems: Prolonged pacifier use, especially beyond the first couple of years, can affect dental development and lead to misaligned teeth.
Increased risk of infections: Pacifiers may contribute to ear infections and thrush, a common yeast infection that occurs in the mouth.
When should I introduce a pacifier to my baby?
The best time to introduce a pacifier depends on your baby’s individual needs and feeding situation.
Breastfed babies: Wait until around 1 month of age, after breastfeeding and latching are well established, before introducing a pacifier. In some cases, your pediatrician may recommend starting sooner if your baby is nursing effectively and gaining weight.
Bottle-fed babies: Babies who drink breast milk or formula from a bottle can typically be introduced to a pacifier at any time, since they don’t need to establish a breastfeeding routine.
Preterm babies: For premature infants, pacifiers can be especially helpful. Non-nutritive sucking supports growth, development, and helps them better transition to oral feeding.
When introducing a pacifier, look for:
The right size, according to your baby’s age.
Pacifiers with one piece, not multiple pieces.
A pacifier that’s easy to clean.
Do pacifiers lower the risk of sudden infant death syndrome (SIDS)?
Pacifier use has been linked to a lower risk of SIDS, which is most common in babies under one year old. Experts aren’t entirely sure why pacifiers reduce SIDS risk, but a few theories exist. One possibility is that babies don’t sleep as deeply when using a pacifier, making it easier for them to wake up if there’s a breathing issue. Another theory is that the pacifier’s position helps keep the tongue forward, preventing it from blocking the airway.
If you have questions about colic or pacifier use, reach out to your local or Summer Health lactation specialist for support. Summer Health is a pediatric telehealth platform offering 24/7 care, providing answers for everything from urgent concerns to everyday questions about your child’s health.

FAQs
What’s the best type of pacifier for babies with colic?
There’s no specific “colic pacifier” proven to treat colic, but certain features improve soothing, such as:
Orthodontic nipple shape: Supports natural palate oral development and is easier to keep in the mouth.
One-piece silicone design: Safer (no seams or parts that can break), easier to clean, and recommended by the American Academy of Pediatrics (AAP).
Soft, flexible medical-grade silicone: May be more comfortable for fussy or colicky infants.
Lightweight shield: Pacifiers with lightweight shield better stay in the mouth, which can be especially helpful with younger infants who fatigue easily.
What’s the best way to clean a pacifier?
Clean your baby’s pacifier with warm water and gentle dish soap. Some pacifiers can be sterilized as well. Always follow the manufacturer’s cleaning instructions for best and safest results. Do not use a pacifier that is damaged.
Is it safe to dip a pacifier in honey or juice?
It is not safe to dip your baby’s pacifier in honey or juice. Honey is dangerous for babies under one year, as it may be contaminated with toxic bacteria called Clostridium botulinum, which may cause infant botulism. Infant botulism is a serious life-threatening disease which can cause damage to the nervous system and death. Additionally, babies do not need sugar from juice, which may also reinforce unhealthy habits and cause oral health issues.
References
Child: care, health and development. A randomized controlled trial of burping for the prevention of colic and regurgitation in healthy infants. https://doi.org/10.1111/cch.12166
The Cochrane database of systematic reviews. Non-nutritive sucking for increasing physiologic stability and nutrition in preterm infants. https://doi.org/10.1002/14651858.CD001071.pub3
Pediatrics. SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment. https://doi.org/10.1542/peds.2016-2938
Child: care, health and development. A randomized controlled trial of burping for the prevention of colic and regurgitation in healthy infants. https://doi.org/10.1111/cch.12166
The Cochrane database of systematic reviews. Non-nutritive sucking for increasing physiologic stability and nutrition in preterm infants. https://doi.org/10.1002/14651858.CD001071.pub3
Pediatrics. SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment. https://doi.org/10.1542/peds.2016-2938
Child: care, health and development. A randomized controlled trial of burping for the prevention of colic and regurgitation in healthy infants. https://doi.org/10.1111/cch.12166
The Cochrane database of systematic reviews. Non-nutritive sucking for increasing physiologic stability and nutrition in preterm infants. https://doi.org/10.1002/14651858.CD001071.pub3
Pediatrics. SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment. https://doi.org/10.1542/peds.2016-2938
Summer Health offers fast and reliable pediatric urgent care through online doctors, all via text. Whether you’re worried about your baby's fever, rashes, or other children's health concerns, we provide expert advice and support anytime, right from your phone.

Never miss a post!
Sign up for our newsletter to receive articles and guides directly to your inbox!

















